VIGILANCE IN ENDOSCOPE REPROCESSING – ISSUE NO. 478
August 1, 2018
Recently, there have been several articles published that highlight the need for continued vigilance in endoscope reprocessing, verification of manual cleaning steps, inspection of endoscopes and follow-up of patients. According to two of these studies, infection rates after endoscopy are higher than previously thought or reported.
This week I sat down with Betty McGinty RN,MSHSA, CGRN, CER , who is the High-Level Disinfection Safety and Quality Director at Northside Hospital in Atlanta to discuss these topics and to have her elaborate on the quality system that she has established in her facilities for endoscope reprocessing. According to Betty, we must pay attention to all infection prevention practices, especially those related to endoscope reprocessing. The message she wanted to convey were these important points:
* There is a need to ensure reprocessing vigilance through initial education, comprehensive education and auditing reprocessing staff throughout the year, not just at annual competency time. Betty recommends that this be done by performing monthly or bi-monthly tracers. Since staff is under so much pressure in facilities to turn scopes around, we need to be watching to ensure compliance.
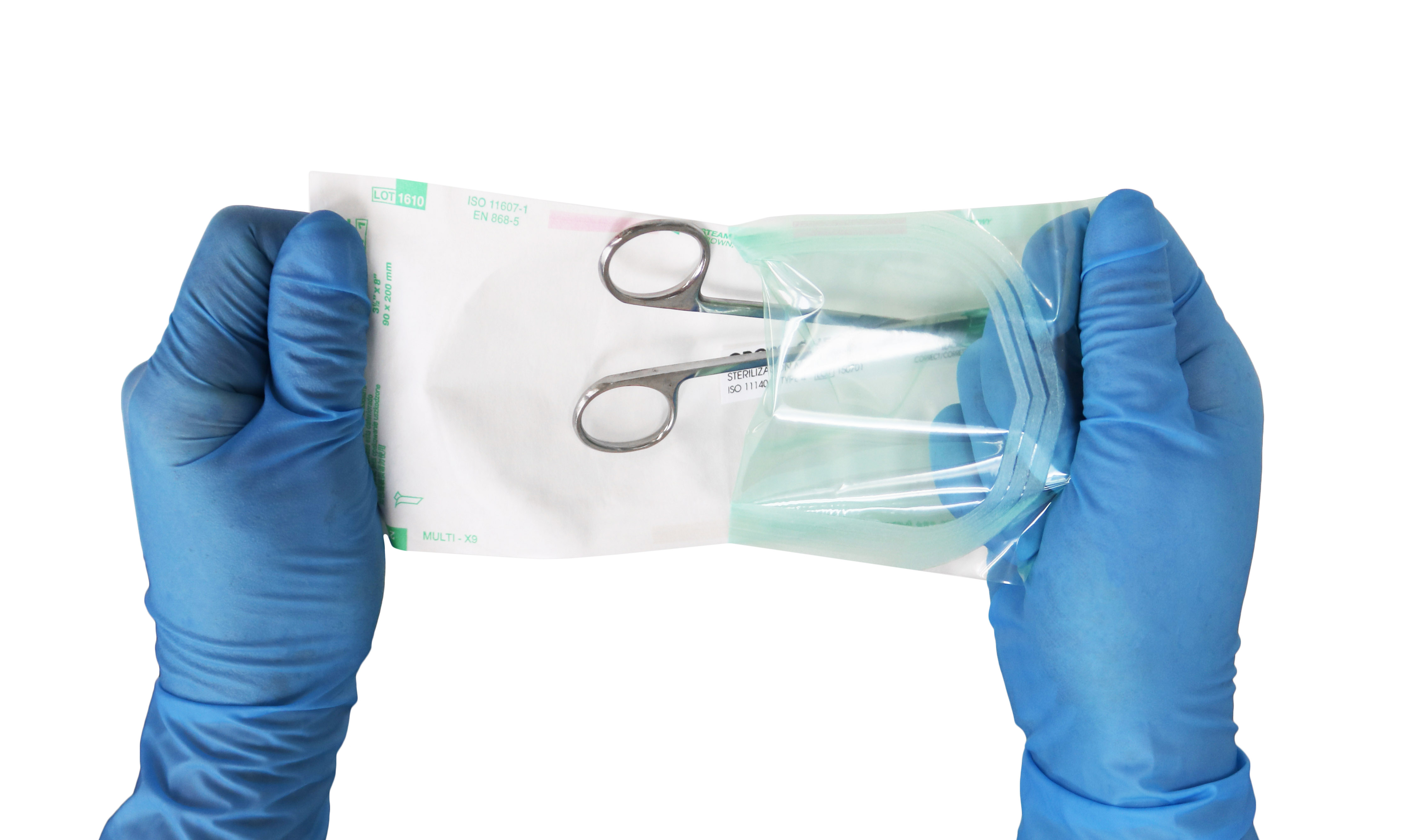
* It is imperative to verify cleanliness prior to high-level disinfection by performing tests for residual contamination, such as tests for protein, hemoglobin or ATP. A facility must decide what type of test the staff will be able to be compliant with and what suits the needs of the facility. Cleaning verification tests need to show the staff whether their cleaning has been effective in order to provide that feedback mechanism. Currently, this step is recommended in standards, but the frequency of performing this step is not agreed upon. At Northside, Betty has chosen to test every scope every time because it is a standard of care issue. SGNA calls this step of cleaning verification the "time out" or safety stop to ensure that cleaning has been performed adequately.
* It is necessary to spot-check endoscopes post-reprocessing for disinfection effectiveness, but what does this mean? At Northside, this is performed with an enzymatic test for gram-negative organisms, called the NOW! test. Endoscopes are tested for gram-negative organisms after reprocessing to determine that they are not contaminated with these high-concern organisms. At Northside, Betty has decided to extend this testing also to ultrasonic probes too as a spot test for residual contamination. A positive result with this test indicates that there is a failure with the disinfection process and closes the loop on the process.
* There is a need to check for the presence of moisture with a borescope. As part of Betty's quality program, a program was established to periodically inspect endoscopes internally for residual moisture. By internal inspection, a facility can verify their drying process is adequate. If moisture is seen, then drying time needs to be increased. SGNA states that, "Drying is a critical element in reprocessing. Moisture allows microorganisms to survive and multiply; therefore, all channels and the surface of the endoscope must be thoroughly dried before storage." Furthermore, SGNA states that an endoscope that is not dry must be reprocessed before use. That is powerful wording!
* Facilities should check for damage to endoscopes by internal and external inspection. An internal inspection is performed with a borescope. At Northside, an endoscope that repeatedly fails cleaning verification testing is inspected with a borescope for internal damage. External visual inspection is also performed with lighted magnification as part of the evaluation and during the normal endoscope reprocessing.
According to Betty, incorporating all of these steps are part of an important part of establishing a quality program for endoscope reprocessing.
HAVE A QUESTION?
WE ARE HERE TO HELP
Have a question about our products? Contact us today to speak directly to a Healthmark team member or shop our catalog now to request a inquiry